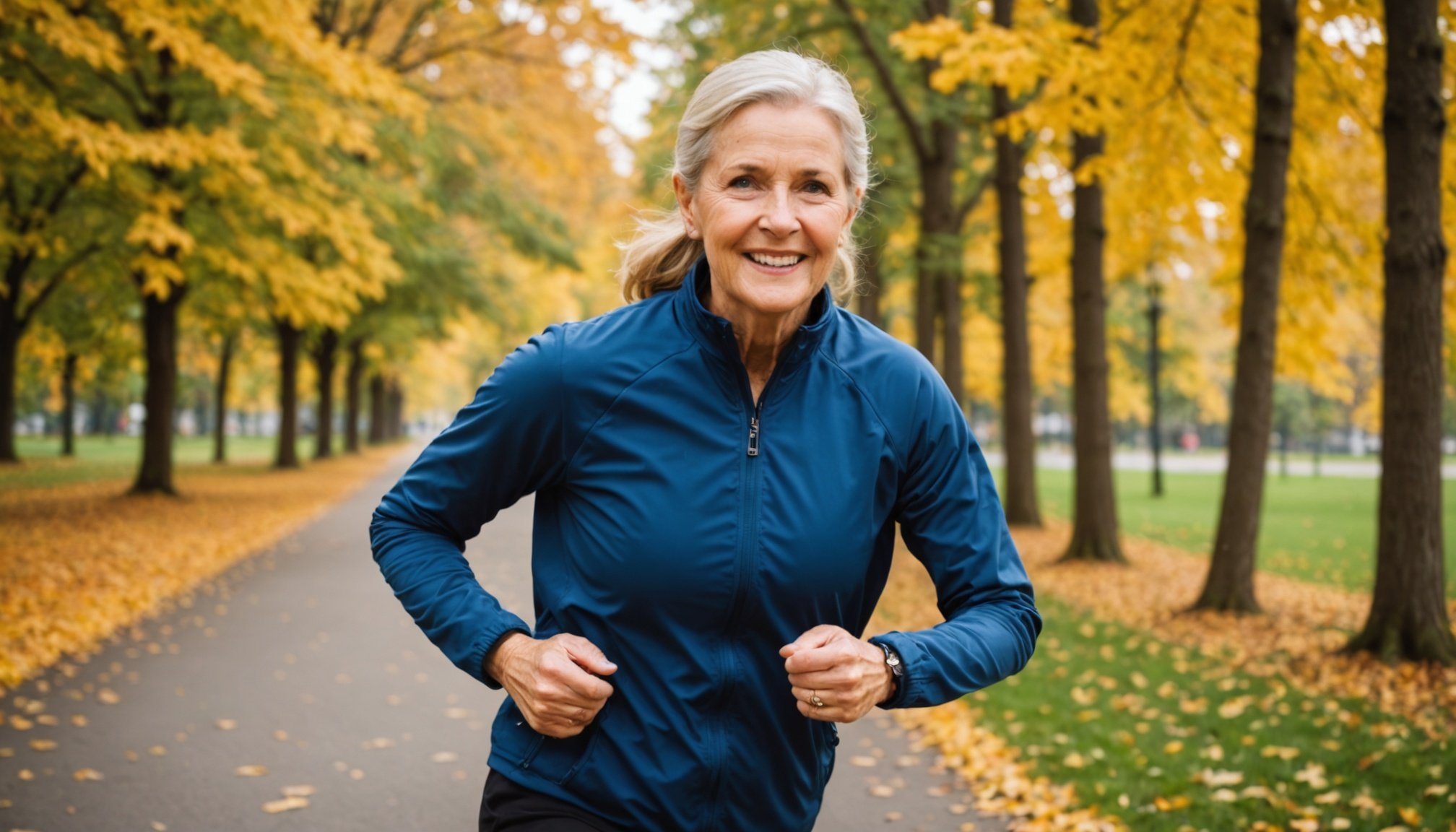
Overview of Osteoporosis and Recovery
Osteoporosis is a condition characterised by weak and brittle bones, increasing the risk of fractures. It affects millions globally, predominantly postmenopausal women, but also men and younger individuals under certain conditions. Recovery strategies are crucial in managing osteoporosis, aiming to improve bone density and reduce fracture risk.
Recovery strategies in osteoporosis encompass a range of approaches, from medication and dietary changes to lifestyle modifications. Physical activity plays a pivotal role in this process, offering significant benefits. Regular exercise, particularly weight-bearing and resistance training, is known to stimulate bone formation and slow bone loss. This is because physical activity influences bone metabolism positively, enhancing bone strength and overall health.
In parallel : Unlocking Relief: The Impact of Plant-Based Supplements on Menstrual Disorder Symptoms
The impact of physical activity can’t be overstated. By integrating exercises like walking, dancing, or low-impact aerobics into regular routines, individuals can improve their mobility and reduce falls, a common concern in osteoporosis. Engaging in physical activities not only contributes to recovery but also enhances quality of life, making it a vital component of osteoporosis management. Tailoring activity levels to individual capabilities ensures safety and maximises benefits, promoting sustainable recovery.
Evidence-Based Physical Activity Interventions
In developing evidence-based interventions to tackle osteoporosis, incorporating various physical activities is essential. Here, we explore effective strategies and practices vetted through research.
Have you seen this : Understanding emetophobia: break free from the fear of vomiting
Weight-Bearing Exercises
Weight-bearing exercises are pivotal for enhancing bone mineral density, pivotal in countering osteoporosis. Activities such as brisk walking, dancing, and hiking apply pressure to bones, stimulating growth. For best results, individuals should engage in these exercises at least three times a week. One real-world example is a community program where participants reported increased bone density after consistent participation in hiking groups.
Resistance Training
Resistance training plays a significant role in maintaining muscle strength, which directly supports bone health. Implementing a safe resistance training routine involves lifting weights or using resistance bands, ensuring correct posture and gradual progression. Research underscores regimes with a minimum of two weekly sessions; one case study noted impressive improvements in both muscle and bone health with structured resistance programs among elderly participants.
Balance and Flexibility Exercises
Balance exercises, such as Tai Chi or standing on one leg, are crucial in fall prevention, a significant risk for individuals with osteoporosis. Flexibility exercises contribute to overall mobility, making daily activities easier and safer. Practical examples include yoga sessions focusing on deep stretches and core stability, showcasing their effectiveness in maintaining mobility. These activities collectively foster an active, osteoporosis-resilient lifestyle.
Research Findings on Physical Activity and Patient Outcomes
Research has consistently linked physical activity to enhanced patient outcomes, particularly in individuals recovering from conditions like osteoporosis. Key studies underline the positive impact of structured exercise regimes on improving recovery timelines and overall quality of life for these patients.
For example, one study demonstrates that osteoporosis patients engaging in regular weight-bearing exercises have seen an increase in bone density by an average of 1.5% over six months, compared to those who remain inactive. This improvement underscores the role physical activity plays in rehabilitation processes.
Moreover, systematic reviews and meta-analyses provide a wealth of insights into these dynamics. They reveal that individuals participating in regular physical exercises report enhanced mental well-being, reduced pain levels, and increased mobility. Quantitatively, participants have observed a 20% improvement in quality of life metrics compared to non-active counterparts.
Such findings highlight not just the physiological benefits, but also the psychological and emotional advantages that come with integrating physical activity into patients’ recovery plans. These comprehensive analyses reinforce why healthcare providers advocate for including regular, tailored physical exercise as a cornerstone of recovery strategies in osteoporosis and similar conditions.
Implementation Strategies for Healthcare Providers
Implementing successful osteoporosis care requires well-structured strategies. Healthcare providers must focus on well-rounded approaches to patient care that take into account individual needs and professional collaboration.
Creating an Individualized Exercise Plan
Customized exercise plans are paramount in effective osteoporosis care. A patient’s unique health characteristics need thoughtful consideration. Start by performing a comprehensive assessment. Identify areas needing improvement and select exercises accordingly. The plan should be continually adjusted based on the patient’s progress. Use monitoring tools like fitness apps and wearable trackers to assess progress. These resources help ensure adherence and motivate patients on their journey to recovery.
Patient Education and Engagement
Educating patients about the importance of physical activity is crucial. Clearly explain how exercise benefits bone health to enhance understanding and motivation. Engaging patients in developing their exercise plans boosts adherence. Offer flexible activity options to cater to varied preferences and overcome barriers like time constraints. Success in patient recovery often hinges on active involvement and education.
Collaboration with Multidisciplinary Teams
The goals of osteoporosis care are more easily achieved through a collaborative approach. Involving a blend of healthcare experts enriches care quality. Physiotherapists, dietitians, and occupational therapists contribute significantly. They offer exercise guidance, nutritional advice, and daily activity modifications. An example is a patient who benefits from a coordinated plan involving strength training, dietary improvements, and ergonomic modifications in their living environment. This illustrates successful multidisciplinary intervention for optimal patient outcomes.
Safety Considerations for Physical Activity in Osteoporosis Patients
Engaging in physical activity is essential for osteoporosis patients but requires careful safety considerations. The risks associated with such activities hinge on bone fragility, increasing the potential for fractures. Patients are encouraged to focus on exercises that build bone strength without exerting harmful stress.
The guidelines for modifying exercises prioritize low-impact activities and emphasize the need for patient safety. For instance, strength training and weight-bearing exercises should be tailored to each individual’s bone density and fracture history. Simple balance exercises or yoga can help improve stability, further minimizing fracture risk.
Undergoing regular evaluations is critical. Healthcare providers can assess bone health progression and adjust physical activity levels to enhance ongoing safety and appropriateness. These evaluations ensure that any changes in bone density or balance capabilities are promptly addressed.
Considerations should also include identifying and eliminating potential hazards in the exercise environment, such as slippery floors or poorly maintained equipment, which could lead to falls. Osteoporosis patients should always communicate openly about their comfort during exercise sessions to avoid further complications.
Incorporating these safety considerations fosters a balanced approach, enabling osteoporosis patients to reap the benefits of physical activity while safeguarding their health.